The human microbiome, a vast ecosystem of trillions of microorganisms living in and on our bodies, has emerged as a focal point of cutting-edge medical research. At the forefront of this microbial frontier is the gut microbiome, home to the largest and most diverse community of these tiny inhabitants. Recent studies have revealed that these microscopic tenants play crucial roles in digestion, immune function, mental health, and even behavior. This paradigm shift in our understanding of human biology is revolutionizing approaches to healthcare, nutrition, and disease prevention. As we unravel the complex relationships between our bodies and our microbial partners, we are discovering new pathways to wellness and redefining what it means to be human.
The concept of the human microbiome has roots dating back to the late 19th century when scientists first observed bacteria in the human gut. However, it wasn’t until the advent of advanced DNA sequencing technologies in the early 21st century that researchers could fully appreciate the diversity and complexity of these microbial communities. The Human Microbiome Project, launched in 2008, marked a turning point in microbiome research, providing a comprehensive map of the microorganisms inhabiting various sites in the human body.
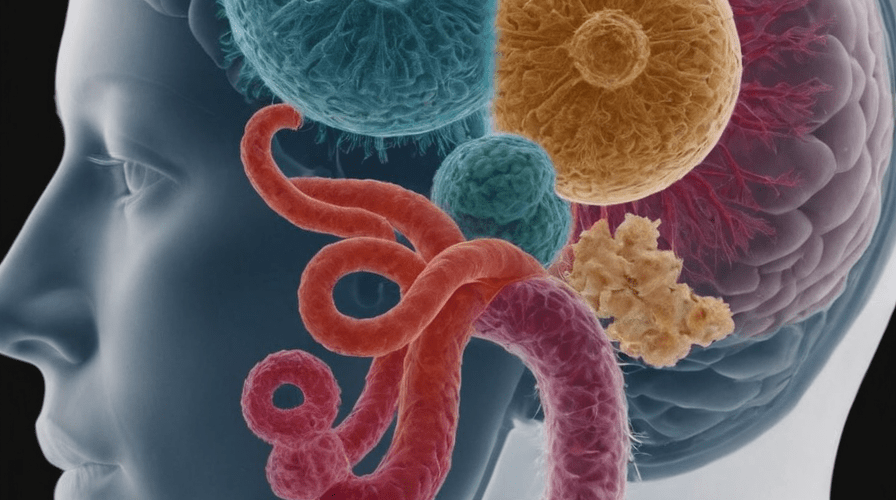
What scientists discovered was astounding: the human body hosts approximately 38 trillion microbial cells, slightly outnumbering our own human cells. These microorganisms, primarily bacteria but also including fungi, viruses, and archaea, form intricate ecosystems within us, with the gut harboring the most diverse and populous community.
The gut microbiome, in particular, has captured the attention of researchers due to its profound influence on human health. This complex community of microorganisms in our digestive tract plays a vital role in breaking down food, synthesizing vitamins, and producing essential compounds that our bodies cannot make on their own. For instance, certain gut bacteria ferment dietary fiber to produce short-chain fatty acids, which serve as a primary energy source for colon cells and have anti-inflammatory properties.
Beyond digestion, the gut microbiome has been found to interact extensively with our immune system. It’s estimated that about 70% of our immune cells reside in the gut, and the microbiome plays a crucial role in training and modulating immune responses. This interaction begins at birth, with the initial colonization of an infant’s gut shaping the development of their immune system. Research has shown that disruptions in this process, such as C-section births or early antibiotic use, may increase the risk of allergies and autoimmune disorders later in life.
Perhaps one of the most surprising discoveries in microbiome research is the gut-brain axis – a bidirectional communication system between the gut microbiome and the central nervous system. This connection helps explain the long-observed link between digestive issues and mental health conditions. Studies have shown that the gut microbiome can influence neurotransmitter production, affect stress responses, and even play a role in conditions such as depression, anxiety, and autism spectrum disorders.
The implications of these findings are far-reaching. In the realm of mental health, researchers are exploring the potential of psychobiotics – live bacteria that, when ingested in adequate amounts, may have a positive effect on mental health. Early studies have shown promising results in using specific probiotic strains to alleviate symptoms of depression and anxiety.
In the field of nutrition, the microbiome is reshaping our understanding of diet and its impact on health. The concept of personalized nutrition is gaining traction, with researchers suggesting that the optimal diet for an individual may depend on their unique gut microbiome composition. This idea challenges the one-size-fits-all approach to dietary recommendations and opens up new possibilities for tailored nutritional interventions.
The microbiome’s influence extends to weight management and metabolic health. Studies have shown that the composition of gut bacteria differs between lean and obese individuals, and that transplanting gut bacteria from lean mice to obese mice can lead to weight loss in the recipients. This has led to research into microbiome-based therapies for obesity and metabolic disorders.
In the realm of infectious diseases, understanding the microbiome has led to innovative treatments. Fecal microbiota transplantation (FMT), once considered a fringe therapy, has become a standard treatment for recurrent Clostridioides difficile infections. This approach, which involves transplanting fecal matter from a healthy donor to restore a patient’s gut microbiome, has shown remarkable success rates and is now being explored as a potential treatment for other conditions, including inflammatory bowel diseases and even certain neurological disorders.
The microbiome’s role in cancer has also become a subject of intense study. Researchers have found that certain gut bacteria can influence the effectiveness of cancer immunotherapies, potentially explaining why some patients respond better to these treatments than others. This discovery has opened up new avenues for enhancing cancer treatments through microbiome modulation.
As our understanding of the microbiome grows, so does the potential for new diagnostic tools. Researchers are exploring the use of microbiome profiles as biomarkers for various diseases, potentially allowing for earlier detection and more personalized treatment approaches. Some scientists even envision a future where routine microbiome testing becomes as common as blood tests in preventive healthcare.
The microbiome revolution is also challenging our concept of what it means to be human. With microbial cells outnumbering our own, some researchers argue that we should view ourselves not as individuals, but as complex ecosystems. This perspective shift has philosophical implications, blurring the lines between self and non-self and raising questions about identity and individuality.
However, as with any rapidly evolving field of science, microbiome research faces challenges and limitations. The complexity of microbial communities and their interactions with the human body makes it difficult to establish clear cause-and-effect relationships. Many studies to date have been correlational, and more research is needed to fully understand the mechanisms by which the microbiome influences health and disease.
Moreover, the microbiome field has seen its share of hype and overblown claims. The market for probiotics and microbiome-based products has exploded, often outpacing the scientific evidence. Consumers should approach such products with caution, as the effects of probiotics can be highly strain-specific and may not provide the broad benefits often claimed.
Looking to the future, microbiome research holds immense promise for revolutionizing healthcare. Scientists are exploring the potential of engineered probiotics as a new class of living medicines, capable of sensing and responding to conditions within the body. Others are investigating the use of phage therapy – using viruses that infect bacteria – as a precision tool for modulating the microbiome.
The concept of the “second genome” – referring to the collective genomes of our microbial inhabitants – is gaining traction in personalized medicine. Just as human genome sequencing has opened up new avenues for tailored treatments, microbiome profiling could lead to highly individualized therapeutic approaches.
As we continue to unravel the complexities of the human microbiome, it’s clear that we are on the cusp of a new era in health and medicine. The recognition of our bodies as complex ecosystems, rather than isolated entities, is transforming our approach to wellness and disease prevention. From personalized nutrition plans to microbiome-based therapies, the possibilities are vast and exciting.
In conclusion, the microbiome revolution represents a fundamental shift in our understanding of human biology and health. As we learn to work with our microbial partners rather than against them, we open up new pathways to wellness that were unimaginable just a few decades ago. The journey of discovery is far from over, and the coming years promise to bring even more groundbreaking insights into the microscopic world within us. In this new frontier of medicine, the key to our health may well lie in the trillions of tiny organisms that call our bodies home.
























Add comment