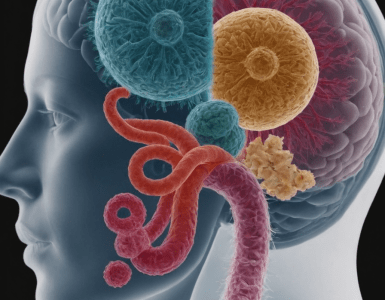
The intricate connection between our digestive system and our brain, known as the gut-brain axis, has emerged as one of the most fascinating areas of medical research in recent years. This bidirectional communication network is reshaping our understanding of mental health, cognitive function, and overall well-being. As scientists delve deeper into this complex relationship, they’re uncovering surprising ways in which our gut health influences our mood, behavior, and even our susceptibility to neurological disorders.
At the heart of the gut-brain axis is the enteric nervous system (ENS), often referred to as our “second brain.” This complex network of neurons lining our gastrointestinal tract can operate independently of the central nervous system and contains more neurons than the spinal cord. The ENS communicates with the brain through the vagus nerve, hormones, and the immune system, creating a constant dialogue between our gut and our mind.
One of the key players in this gut-brain communication is the microbiome – the trillions of microorganisms that inhabit our digestive tract. These bacteria, viruses, and fungi play crucial roles in digestion, immune function, and the production of various neurotransmitters. In fact, about 95% of the body’s serotonin, a neurotransmitter crucial for mood regulation, is produced in the gut.
Research has shown that the composition of our gut microbiome can significantly impact our mental health. Studies have found correlations between certain gut bacteria populations and conditions such as depression, anxiety, and even autism spectrum disorders. For example, individuals with depression often show lower levels of Lactobacillus and Bifidobacterium species in their gut microbiome.
The gut microbiome’s influence extends beyond mood to cognitive function. Emerging research suggests that a healthy, diverse gut microbiome may support better memory and cognitive flexibility. Conversely, imbalances in gut bacteria have been linked to cognitive decline and may play a role in neurodegenerative diseases like Alzheimer’s and Parkinson’s.
Inflammation is a crucial factor in the gut-brain axis. Chronic inflammation in the gut can lead to increased permeability of the intestinal lining, often referred to as “leaky gut.” This allows substances that should remain in the gut to enter the bloodstream, potentially triggering systemic inflammation that can affect brain function. Some researchers believe this mechanism may contribute to the development or exacerbation of neurological disorders.
The gut-brain axis is bidirectional, meaning that not only does our gut influence our brain, but our mental state can also affect our digestive health. Stress, for instance, can alter gut motility, increase intestinal permeability, and change the composition of the gut microbiome. This explains why stress and anxiety often manifest as digestive symptoms like stomach aches or changes in bowel habits.
Diet plays a crucial role in maintaining a healthy gut-brain axis. A diet rich in diverse plant fibers, fermented foods, and omega-3 fatty acids can promote a healthy, diverse gut microbiome. Conversely, diets high in processed foods, sugar, and unhealthy fats can lead to dysbiosis – an imbalance in gut bacteria that may negatively impact mental health.
Probiotics and prebiotics are gaining attention as potential tools for supporting mental health through the gut-brain axis. Probiotics are live beneficial bacteria, while prebiotics are fibers that feed these beneficial bacteria. Some studies have shown promising results in using specific probiotic strains to alleviate symptoms of depression and anxiety, though more research is needed to fully understand their effects.
The gut-brain axis may also play a role in our sleep patterns. The gut microbiome influences the production of melatonin, a hormone crucial for regulating our sleep-wake cycle. Disruptions in the gut microbiome have been linked to sleep disorders, while improving gut health may lead to better sleep quality.
Understanding the gut-brain axis has led to new approaches in treating various conditions. For example, some researchers are exploring the use of fecal microbiota transplants – transferring gut bacteria from a healthy donor to a patient – as a potential treatment for certain neurological and psychiatric disorders.
The implications of the gut-brain axis extend to early life development. The establishment of a healthy gut microbiome in infancy and early childhood may play a crucial role in brain development and long-term mental health. Factors such as mode of birth (vaginal vs. C-section), breastfeeding, and early exposure to antibiotics can all influence the developing gut microbiome and, potentially, future mental health outcomes.
As research in this field progresses, it’s becoming clear that maintaining a healthy gut is crucial for overall well-being, including mental health. Simple lifestyle changes like improving diet, managing stress, getting regular exercise, and ensuring adequate sleep can all contribute to a healthier gut-brain axis.
In conclusion, the gut-brain axis represents a paradigm shift in our understanding of mental health and cognitive function. It highlights the interconnectedness of our bodily systems and underscores the importance of a holistic approach to health. As we continue to unravel the complexities of this fascinating connection, we may discover new ways to support mental health, prevent neurological disorders, and enhance overall well-being through the power of our “second brain” – the gut.























Add comment